Anterior Cruciate Ligament Repair
Contact Us
Request an AppointmentPlease note that a referral letter is required before an appointment can be confirmed.
Please note that a referral letter is required before an appointment can be confirmed.
Useful Information
About this service
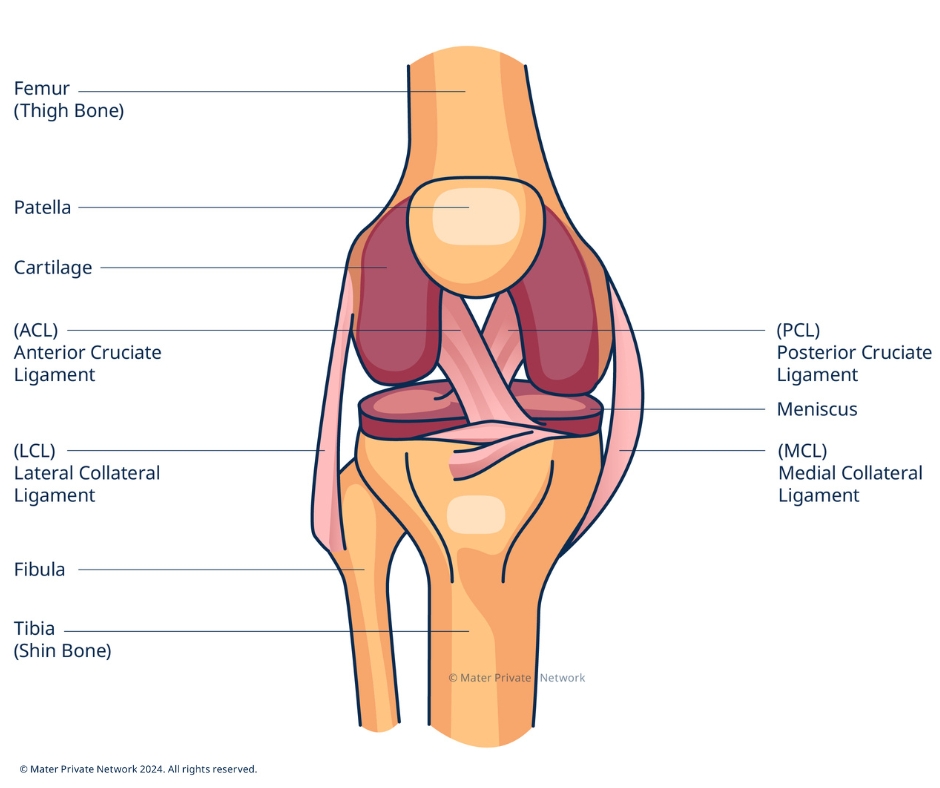
The anterior cruciate ligament (ACL) is one of the most important ligaments in your knee. It prevents excessive forward movement of the tibia relative to the femur and controls rotation of these two bones.
However, your ligament can be relatively easily injured particularly during sports activities, and this injury can be very painful. ACL injuries often happen when you twist your leg while your foot is planted on the ground.
Signs or symptoms that you have an ACL injury include:
- Hearing a ‘pop’ sound when you are initially injured
- Pain in your knee when you put weight on your leg
- Swelling of your knee
- A feeling that your knee is unstable
- Loss of range of motion
Will an ACL injury require surgery?
Whether you need surgery or not will depend on the outcome of your scan. There are three types or grades of injury.
- Grade I sprain: some stretching and micro-tearing of your ACL, but your ligament is intact, and the joint remains stable. These injuries rarely require surgery.
- Grade II sprain (partial disruption): some tearing of your ligament. Your ligament is partially disrupted, and the joint is moderately unstable. Depending on the patient and the degree of instability, these tears may or may not require surgery.
- Grade III sprain (complete disruption): total rupture of your ligament causing your joint to be unstable. Surgery is usually recommended in young or athletic persons who engage in cutting or pivoting sports.
A completely torn ACL will never heal back to its pre-injury state even following rehabilitation and physiotherapy. In addition, even with a partially torn ligament, the normal motion of the knee may be altered.
Additional Complications
ACL injuries can be accompanied by other injuries such as:
- Meniscus tear: menisci are “cushions” between your tibia and femur that act as a shock absorber. A meniscus tear typically occurs with twisting motions.
- Medial collateral ligament (MCL) tear: your MCL provides stability on the inside of your knee. Injury to the MCL is quite common, but if it is an isolated injury, it can usually be treated with physiotherapy and bracing.
How is ACL diagnosed?
The diagnosis of ACL injuries can usually be accurately diagnosed by clinical examination of your knee. If necessary an MRI can be used to diagnose the condition.
There are two different grafts used when repairing the ACL.
The first is a hamstring tendon autograft where one of your five hamstring tendons which help to flex the knee is used to reconstruct the ACL.
The other is a patellar tendon autograft where the middle third of your patellar ligament, that runs from the bottom of the kneecap (patella) to the front of the tibia, is used along with bone blocks from the patella and the tibia. Your consultant will discuss your options and their impact with you in advance of surgery.
The operation takes between one and two hours to complete. After the procedure, you will normally spend one to two hours in a recovery room and can usually be discharged on the same day.
You will be given pain medication to help with the pain and swelling from surgery. You will also be provided with a prescription for pain medication before you are discharged.
During recovery, which can take a few months, your knee must be protected with a postoperative brace to prevent overuse or stressing of the area while the knee heals.
You will also be required to follow a strict rehabilitation program to ensure that your knee heals correctly. Please note that many patients will feel comfortable long before healing has finished but it is essential that you continue to restrict your activity in line with post-operative advice.
ACL reconstruction is usually very effective and if the knee is cared for properly and subsequent traumatic injuries are avoided, the benefits of the surgery should be permanent.
In general, patients can perform gentle activities of daily living starting two or three weeks after surgery. Most people who work at a desk job can return to work during this time. The patient is strongly encouraged to continue wearing a functional knee brace.










