Posterior Lumbar Decompression/Discectomy
Contact Us
Request an AppointmentPlease note that a referral letter is required before an appointment can be confirmed.
Please note that a referral letter is required before an appointment can be confirmed.
Useful Information
About the service
Decompression involves the removal of bone to relieve pressure and pinching of the spinal nerves. Discectomy removes the parts of the disc that are bulging (herniated), causing irritation or compression on the nerve. Decompression and discectomy are frequently performed at the same time.
Lumbar decompression is only recommended when non-surgical treatments (i.e physiotherapy, targeted injections) have not helped to eliminate the pain or other symptoms which are affecting a patient’s quality of life.
Surgery aims to improve symptoms such as persistent pain (sciatica) and numbness (tingling, paraesthesia) in the legs caused by pressure on the nerves in the spine.
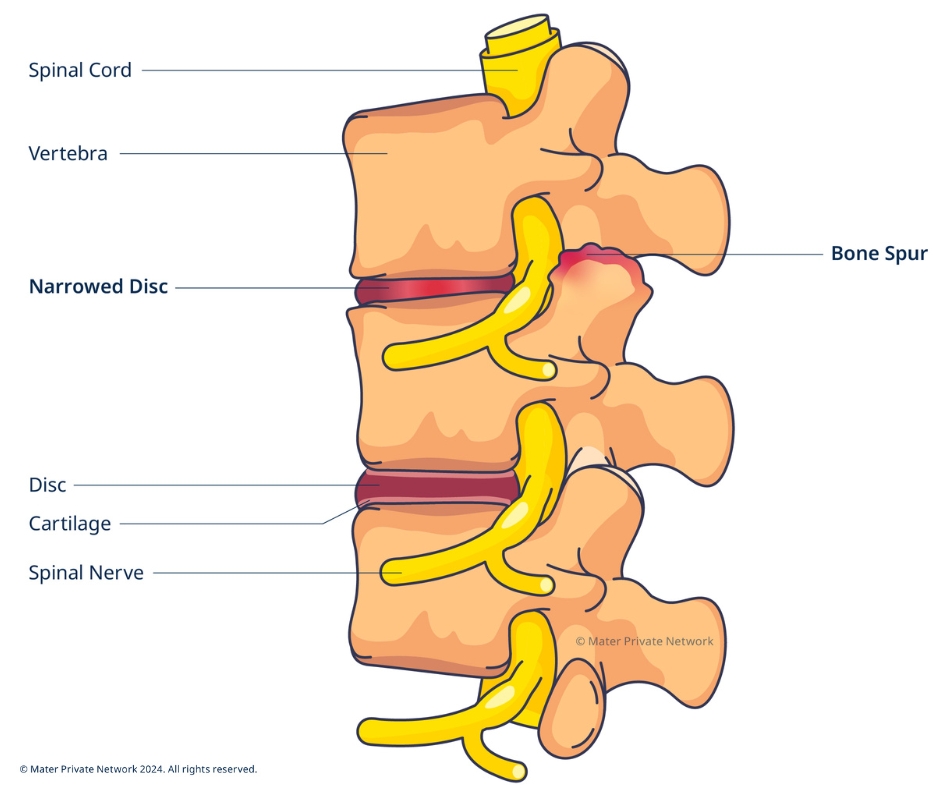
Decompression
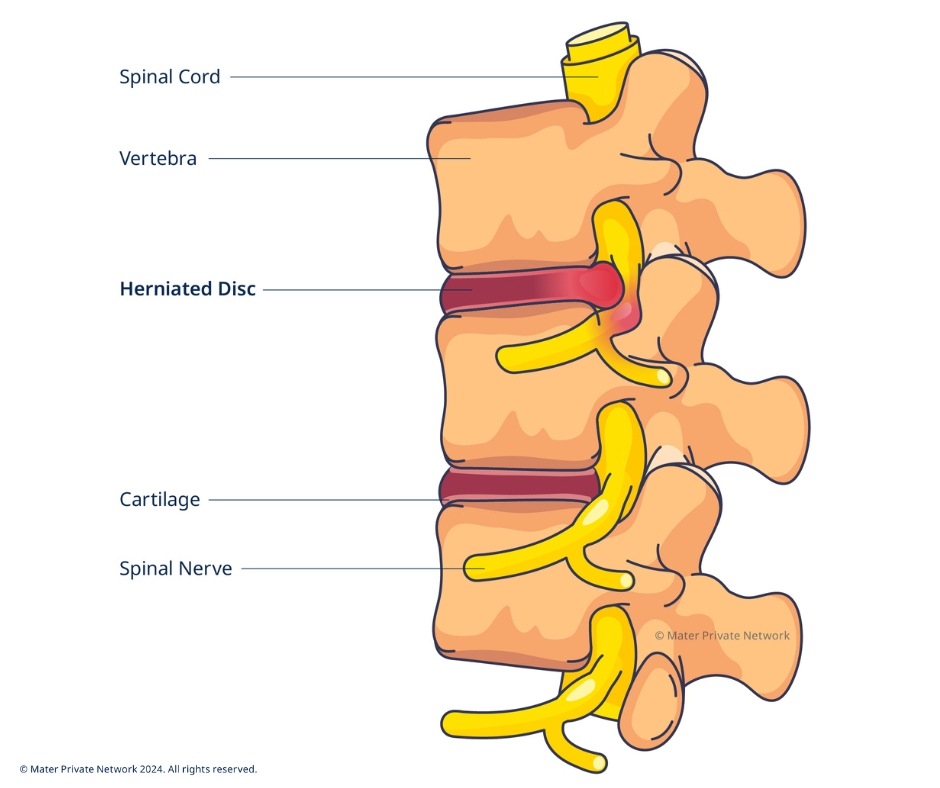
Discectomy
Diagnosis
Your consultant will review your history and current condition, including pain level, flexibility, sensation, and muscle strength.
Imaging such as X-ray, CT or MRI may also be required as part of your diagnosis. Your doctor will take you through what will be involved.
Conditions
Posterior lumbar decompression and discectomy surgery is often used to treat:
- Spinal stenosis – narrowing of a section of the spinal column, which puts pressure on the nerves inside.
- A (herniated) slipped disc and sciatica – where a damaged spinal disc presses down on an underlying nerve.
- Lumbar radiculopathy – a condition causing pressure on the nerve root which causes pain in the lower back and hip, radiating down the back of the thigh into the leg.
What to expect
There are several things you can do to prepare yourself for spinal surgery.
In the weeks before your surgery, it is advisable to eat a balanced diet as this can help the healing process.
If you smoke, stop as far in advance of surgery as possible. Smoking can delay or interfere with healing and may cause complications with the anaesthetic.
Pre-operative assessment clinic
Within one month (ten days - one week) of your surgery, some patients will be invited to attend the pre-operative assessment clinic. The pre-assessment clinic reviews your current health, to confirm your fitness for surgery. During this visit you will be asked about your medical history and any medications you are taking. You will have blood tests done, and may have an electrocardiogram (ECG) and X-ray done. This clinic is an excellent opportunity for you to ask any questions you may have, and to get any information you need to plan for your discharge from hospital and recovery.
During surgery, the bone (overgrowth) and/or disc material causing issues are removed, creating more space to alleviate pressure on the nerve.
Modern surgical techniques are less invasive, which in turn means less trauma to the muscles and ligaments surrounding the area. This results in better, faster healing. Most patients get good relief after surgery, and find their pain is improved.
When your surgery is completed, you will be moved to the recovery room where you will be observed and monitored by a nurse until you awake from the anaesthesia. You will then be transferred to a ward where the ward team will work closely with you to aid your recovery.
- You will have a drip for intravenous fluids through a vein into your arm or hand for a few hours after your surgery.
- When you are fully awake, you may eat and drink, starting with sips of water then a light meal.
- You may also have a catheter inserted into your bladder to make urination easier.
- There may be a drain tube in your back which is normally taken out the day after surgery.
- There is usually some level of pain following spinal surgery. The anaesthetist and nurses will work closely with you to manage your pain.
A physiotherapist/nurse will get you out of bed and on your feet within a few hours after surgery. This is not only safe, but also the best way to get your muscles moving and prevent post-operative complications.
It is important to note that patients are often at increased risk of falls after surgery. The nursing and physiotherapy team will take you through what you need to be aware of, and how to avoid a fall.
Frequently asked questions
In most cases, usually only part of the disc is removed – the part causing problems. However, on occasion the whole disc is removed if required.
With minimally invasive surgery the incision is usually quite small, less than 2 inches.
Discectomy is considered a safe procedure, with many benefits for patients living with debilitating pain, numbness, tingling, and other symptoms. But as with any surgery, there is a risk of complications. Potential complications include:
- Bleeding
- Infection
- Leaking spinal fluid
- Injury to blood vessels or nerves in and around the spine










