Spinal Stenosis
What is spinal stenosis?
Spinal stenosis is a narrowing in the spinal canal, which results in pressure on the spinal cord and nerve roots. It usually develops slowly, and over time, and is a degenerative condition.
Symptoms are not always obvious or apparent immediately, often they are assumed to be associated with aging or wear-and-tear. Symptoms can include pain, numbing, tingling, poor balance.
Spinal stenosis is most common in the lower back, and occurs in the neck area. It is classified according to where on the spine it occurs.
- Cervical stenosis: where the narrowing is in the part of the spine that’s in your neck.
- Lumbar stenosis: where the narrowing is in the part of the spine in your lower back.
There are many causes of spinal stenosis, the most common being osteoarthritis. Treatment options include physical therapy, medication, and where appropriate surgery.

Who gets spinal stenosis?
Spinal stenosis usually happens as we age, due to wear and tear. Commonly it would be seen over the age of 50 years. Some people are born with it.
What is the main cause of spinal stenosis?
Spinal stenosis is a degenerative spinal disease, which usually develops over time. The most common cause is damage caused by osteoarthritis.
Other causes include:
- Herniated disks. These shock absorbers between the vertebrae in the spine. With age, they tend to dry out with age and crack, releasing some of the soft inner material, which presses on the spinal cord or nerves.
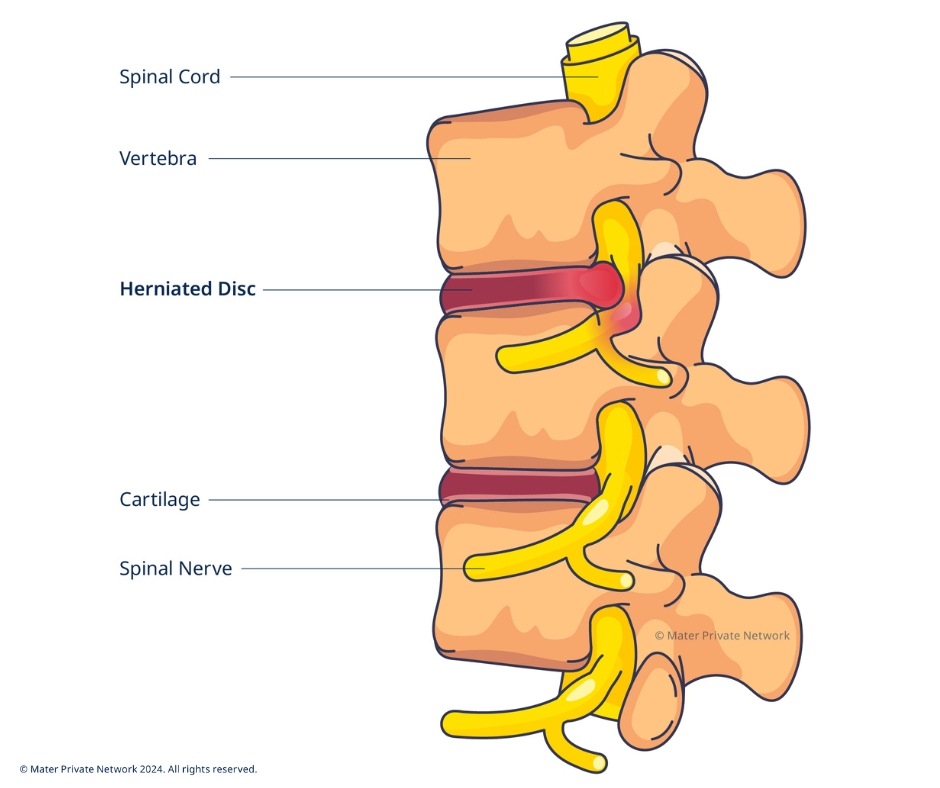
- Thickened ligaments. Ligaments which hold the bones of the spine together, can become stiff and thickened over time, causing them to protrude into the spinal canal.
- Spinal injuries. Accidents and other trauma can cause dislocations or fractures of one or more vertebrae. Displaced bone from a spinal fracture may damage the contents of the spinal canal. Swelling of nearby tissue immediately after back surgery also can put pressure on the spinal cord or nerves.
- Tumours. Abnormal growths inside the spinal cord, within the membranes that cover the spinal cord or in the space between the spinal cord and vertebrae. These are uncommon.
What are the symptoms of spinal stenosis?
Symptoms of spinal stenosis may have been present for a long time, but not bothersome or even noticeable. As the degeneration progresses, the narrowing can press or push in on the spinal cord or nerves, causing them to become irritated, compressed, or pinched, resulting in back pain and sciatica.
Symptoms depend on where, and how severe, your spinal stenosis is. You might symptoms in your neck, back, arms, legs, hands and feet:
- Cramping in one or both legs when walking or standing for long periods of time
- Pain
- Numbness
- Tingling
- Loss of balance
- Loss of bladder or bowel control (in severe cases)
When should I see a doctor?
If you have any of the symptoms described above, make an appointment with your GP.
How is spinal stenosis diagnosed?
Your doctor may ask you about symptoms and carry out a physical examination. Some of the common diagnostic tests used include;
- X-rays: an X-ray can show changes to the bone, such as bone spurs.
- Magnetic resonance imaging (MRI): an MRI produces cross-sectional images of your spine and can reveal damage to your disks and ligaments, as well as the presence of tumours. It is also effective in identifying where the nerves in your spinal cord are being constricted.
- CT scan: this test combines X-ray images taken from many different angles to produce detailed, cross-sectional images of your body. In some CT scans a contrast dye is injected which outlines the spinal cord and nerves and can expose herniated disks, bone spurs and tumours.
- Electroencephalogram (EEG): this test helps to evaluate the condition of spinal nerve.
What are the treatments for spinal stenosis?
Treatment for spinal stenosis depends on the location and severity of the stenosis, along with the symptoms you are experiencing.
Non-surgical approaches
Mild cases of stenosis may be treated with non-surgical approaches to control symptoms, including:
- Exercise: certain exercises can help relieve your pain, strengthen the muscles, and provide necessary support to your spine.
- Lifestyle changes: identifying and adjusting activities, positions and postures that worsen your symptoms. Diet changes to reduce and manage weight, if it is a factor. Looking at sleep, diet, and smoking to improve overall health and well-being
- Hot treatments: hot treatments can relieve pain experienced from conditions such as osteoarthritis by relaxing the muscles and relieving the joints. Remember to be cautious when applying hot treatments and be mindful not to burn yourself.
- Cold treatments: if you find that the hot treatments do not work well for you, cold treatments can reduce swelling, tenderness and inflammation.
- Physiotherapy: your physiotherapist will be able to advise you on the best exercises to relieve your pain and, to improve your strength and balance.
- Steroid injections: injections can help reduce inflammation and pain.
- Pain relief medication: your consultant or GP will be able to advise you on mediation options, both over-the-counter and prescription.
Surgery
Surgery is more likely to be considered for advanced stenosis, and when other treatment options are no longer providing relief.
Laminectomy: laminectomy involves the removal of the lamina, which is the back portion of the vertebrae covering the spinal canal, usually associated with symptoms caused by arthritis.
Spinal fusion: spinal fusion connects two or more parts of bone together to provide strength, stability, and support.
Mater Private Network in Dublin is the only Irish hospital to offer robotic-assisted spinal fusion surgery. Advanced robotic technology improves visualisation and precision during surgery. This has many benefits for patients including smaller incisions, reduced blood loss, and faster recovery.
Frequently asked questions
Can I walk if I have spinal stenosis?
Yes, walking is a good exercise for spinal stenosis. If you find it difficult to walk due to pain or imbalance, please discuss this with your consultant or physiotherapist.
Can you cure spinal stenosis?
Unfortunately, there is nothing you can do to stop the progression of spinal stenosis. However, different types of treatments will help relieve the symptoms.
Are spinal stenosis and sciatica the same?
Sciatica is a symptom of spinal stenosis. However, not all patients with spinal stenosis will experience sciatica.