Colporrhaphy (Vaginal Wall Repair)
Contact Us
Request an AppointmentPlease note that a referral letter is required before an appointment can be confirmed.
Please note that a referral letter is required before an appointment can be confirmed.
Useful Information
About Colporrhaphy (Vaginal Wall Repair)
Colporrhaphy is a surgical procedure to reinforce the vaginal walls and treat pelvic organ prolapse (POP).
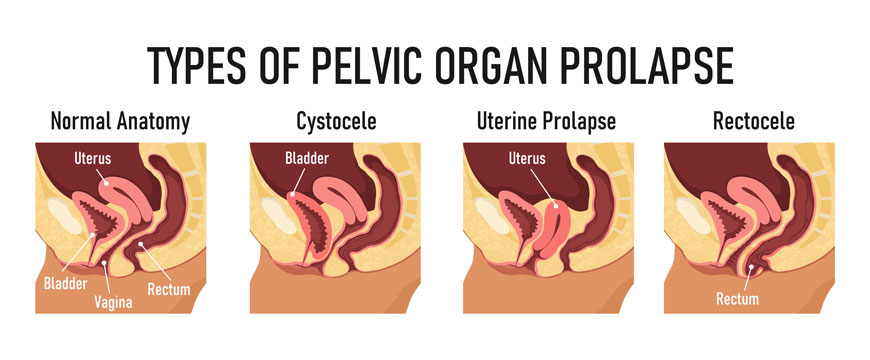 Anterior vaginal wall prolapse is when your bladder protrudes against the front wall of your vagina. It can sometimes feel like a bulge coming out through the vaginal opening. It is also known as cystocoele. About 10% of people who have had children
will require surgery, such as colporrhaphy, for anterior vaginal prolapse.
Anterior vaginal wall prolapse is when your bladder protrudes against the front wall of your vagina. It can sometimes feel like a bulge coming out through the vaginal opening. It is also known as cystocoele. About 10% of people who have had children
will require surgery, such as colporrhaphy, for anterior vaginal prolapse.
Posterior vaginal wall prolapse is when there is a bulge or a sensation of ‘something coming down’ from back wall of the vagina. This is also known as rectocele. About 10% of people will require surgery, such as colporrhaphy, for posterior vaginal wall prolapse.
Colporrhaphy strengthens the muscles and tissues in your vaginal wall so that they can support your pelvic organs. There are two types of colporrhaphy – posterior colporrhaphy and anterior colporrhaphy.
What is Posterior Colporrhaphy?
Posterior colporrhaphy (posterior vaginal wall repair) is a procedure to treat prolapse of the back wall of the vagina (rectocele). It reinforces the tissue between the rectum and the vagina. Another procedure called perineorrhaphy repairs the perineal body and helps to support the back wall of the vagina.
What is Anterior Colporrhaphy?
Anterior Colporrhaphy (anterior vaginal wall repair) is a procedure used to treat prolapse of the front wall of the vagina (anterior vaginal wall prolapse). Behind this wall sits the bladder and urethra.
What are the benefits of Anterior and Posterior Colporrhaphy?
80-90 % of patients having surgery for posterior vaginal wall prolapse find it successful, with approximately 50% of patients who experienced incomplete bowel emptying or constipation reporting an improvement after surgery. 70-90% of patients find anterior colporrhaphy successful. With both conditions, there is always a chance that the prolapse may return in the same or a different part of the vagina, however by following the discharge advice this is less likely to occur.
Alternatives to surgery
There are alternatives to surgery although the alternatives are not suitable for everyone. If you decide not to have surgery, or to wait, the alternatives include:
- Doing nothing
- Vaginal pessaries
- Vaginal laser
Your doctor will discuss with you the suitable alternatives and options available to treat your own specific symptoms.
Before going ahead with surgery, your doctor will perform a pelvic exam and any additional tests needed to evaluate your condition.
Prior to surgery, fasting will be required. Your doctor will discuss this and any other instructions prior to surgery.
Colporrhaphy is usually carried out under general anaesthesia so you will be asleep during the procedure. An incision will be made to access and repair the weakened tissue. Using absorbable stitches, the bladder and urethra, or rectum, are repositioned to their correct location, and any excess tissue is removed.
With anterior colporrhaphy, once the repair is complete, a cystoscopy will be carried out to check the bladder. A cystoscopy is a test using a small camera which is inserted inside the bladder, giving your surgeon the chance to look inside.
With posterior colporrhaphy, the perineal body is also repaired, as required, by placing stitches into the perineal muscles to help build up and support the perineal body.
You may have some pain, but this can be managed with regular pain killers. A specialised vaginal bandage known as a vaginal pack will be in place for 24- 48 hours after surgery. The vaginal pack provides pressure to the vaginal area to help with reducing bleeding.
During your initial recovery a catheter (small tube in your bladder) will be in place to help you to empty urine without having to go to the toilet. When the catheter is removed, your bladder will be checked to ensure that it is emptying correctly.
Typically, patients stay in hospital for 2 nights. Your consultant will advise you on your expected length of stay.
Generally, you should allow 6 weeks for recovery.
You will need to avoid heavy lifting, strenuous activity, constipation, and sexual intercourse for six weeks after the procedure to allow your body to heal properly.
With regards to driving it is always important to check with your insurance provider. Usually, most drivers are safe to resume driving 4-6 weeks after surgery as long as a full emergency stop can be performed without hesitation.
You will be given a discharge summary and a copy will be sent to your GP.
You will need to be collected from the hospital. Ideally you should have a family member or friend that is able stay with you or regularly check in during the first week.
If necessary, a prescription for any additional medication will be given to you on discharge.
If you have any concern after discharge, please call your consultant’s secretary during office hours, or contact your GP or the hospital. In the event of an emergency, at any time, please contact or go directly to the Emergency Department at your nearest local hospital.
Follow your discharge instructions. There is always a chance that the prolapse may return in the same or a different part of the vagina, however by following the discharge advice this is less likely to occur.
For the first 6 weeks avoid the following to allow your body to heal properly:
- using tampons
- sexual intercourse
- constipation
- heavy lifting
Move as much as you are able every day, try to increase this slightly every week.
Maintain a high fibre diet and keep hydrated. Constipation can contribute to posterior vaginal wall prolapse, so it is important to try and avoid developing constipation.
Allow plenty of time to rest each day.
On occasion, anterior vaginal wall prolapse treatment can unmask urinary incontinence, which may require further investigation and management.
Remember you have had surgery, while it is important to be active in your recovery, listen to your body.