Vulval Cancer
I’ve been told that I have vulval cancer. What is it exactly?
Cancer of the vulva is also known as vulval or vulvar cancer. Cancer of the vulva is very rare and in Ireland, less than 40 women are diagnosed with it each year. The vulva is the outer part of the vagina. The most common areas in which this cancer forms are the outer lips (labia majora) and inner lips (labia minora) but less commonly in the clitoris. 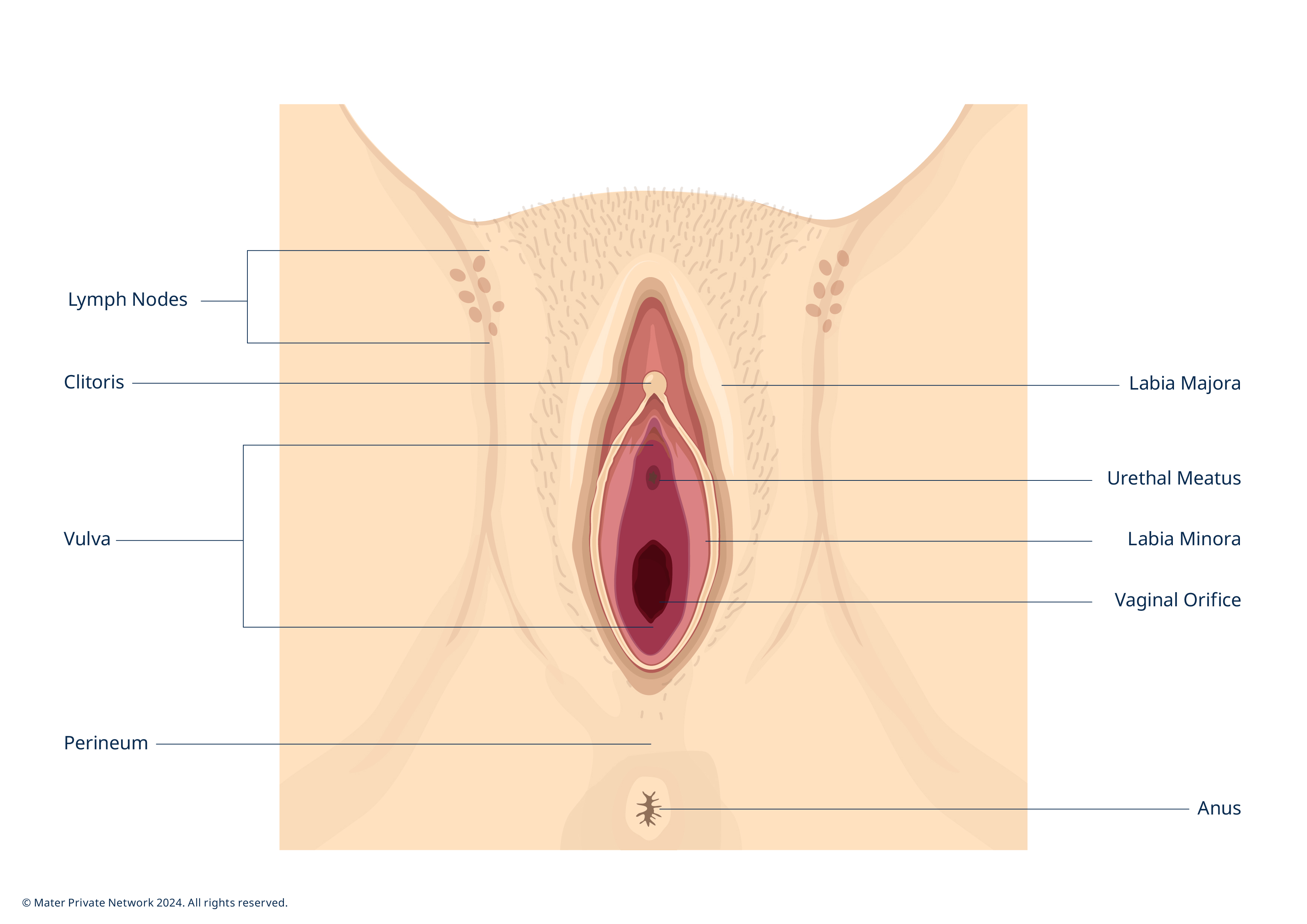
The exact cause of vulval cancer is unknown. However, there are risk factors that can increase your chance of developing the condition:
- VIN: vulval intraepithelial neoplasia causes cell changes in the skin of the vulva. It is linked to the human papilloma virus (HPV). VIN is not a cancer but is precancerous and if left untreated can lead to vulval cancer.
- Age: most vulval cancers are diagnosed in women over 55 years of age.
- Smoking: smoking may also increase the risk of developing both VIN and vulval cancer. The chemicals in cigarettes can affect how you fight infection in the vulva.
- Benign conditions: if you have certain skin conditions for a long time, you have a higher risk of developing vulval cancer. These conditions include vulval lichen sclerosus and vulval lichen planus. Both can cause long-term inflammation of the skin in the vulval area.
There are different types of vulval cancer, some of which are very rare. They include:
- Squamous cell carcinoma
- Adenocarcinoma
- Vulval melanoma
- Verrucous carcinoma
- Sarcoma
What are the symptoms of vulvar cancer?
Often vulval cancer does not cause any early symptoms. The most common symptoms are:
- Itching, burning and soreness of the vulva
- A lump, swelling or wart-like growth on the skin of the vulva
- Thickened, raised, red, white or dark patches on the skin of the vulva
- Bleeding or a blood-stained vaginal discharge
- Burning pain on passing urine
- Pain in the vulva
How is vulval cancer diagnosed?
How gynaecological cancer is diagnosed depends on what type of cancer is suspected. Pelvic exams, imaging tests, biopsies, colposcopy exam and possible diagnostic surgery are all methods of diagnosing gynecological cancer.
Once cancer is confirmed, the stage of the cancer is determined and a treatment plan is developed. Staging refers to how far the cancer has spread to nearby tissue or organs. Among each of the various types of gynaecological cancer, early detection is crucial. However, detection can be very difficult, especially in the early stages.
Tests such as the following may be used for diagnosis:
- Transvaginal ultrasound: an ultrasound used to build up a picture of the tissues in your womb. During a transvaginal ultrasound a small metal ‘probe’, covered with a gel is inserted into the vagina. This creates the images for the scan. This test is not painful but may be a little uncomfortable.
- Hysteroscopy: a hysteroscope is a thin, flexible tube with a light at the end which is passed through the vagina and into the womb. This allows the doctor to look inside the womb and take tissue samples or a biopsy.
- Biopsy: a small amount of tissue samples are taken from the womb during a hysteroscopy. Biopsies are sent to a laboratory and looked at under a microscope to detect if cancer cells are present.
- D&C - dilatation and curettage: during a D&C the cervix and entrance to the womb are gently opened. Samples of tissue from the inner lining of the womb are taken with an instrument shaped like a spoon called a curette. The samples are then sent to the laboratory to be examined.
What is the treatment for vulvar cancer?
Your doctor will plan your treatment based on the stage of the cancer, your age and general health. The main treatments for vulval cancer are:
- Chemotherapy
- Radiotherapy
- Surgery
The aim of surgery is to remove the cancer. The type of surgery depends on the size and position of the cancer. There are different types of surgery available including:
- Wide local excision - in this surgery, the cancer cells are removed as well as an additional border area of 1cm, to ensure all cells are removed.
- Radical local excision - in this surgery, the cancer and a larger border are removed. Lymph nodes may also be removed.
- Partial vulvectomy - involves removal of part of the vulva.
- Total or radical vulvectomy - removal of the entire vulva and the surrounding lymph glands.
- Pelvic exenteration - if the cancer has spread beyond the vagina, the surgery may involve removing the affected organs, for instance the cervix or part of the lower bowel or bladder.









