Pelvic Organ Prolapse
What is pelvic organ prolapse?
Pelvic organ prolapse is a common condition where one or more of the pelvic organs (bladder, uterus or bowel) bulges against the vaginal walls and in some cases can come through the opening of the vagina. This occurs because the tissues, ligaments and muscles in this area have been weakened or over stretched.
Pelvic organ prolapse is more common in women who have had children, experienced vaginal childbirth and/or reached the menopause.
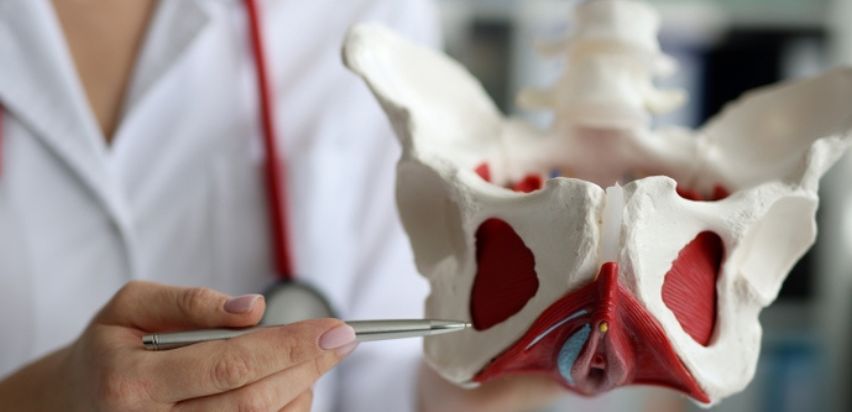
What are the different types of prolapse?
Depending on what organ is involved, there are several different types of pelvic organ prolapse.
- Vault prolapse: the top of the vagina drops down into the vaginal canal, this occurs in women who have had a hysterectomy (removal of uterus and cervix).
- Uterine prolapse: the uterus falls into the vagina, sometimes protruding out of the vaginal opening.
- Cystocele: the bladder protrudes against the front wall of the vaginal and can sometimes feel like a bulge coming out through the vaginal opening.
- Urethrocele: the urethra (the tube which empties urine form the bladder) pushes against the front wall of the vagina.
- Rectocele: the rectum protrudes into the back wall of the vagina and can sometimes feel like a bulge coming out through the vaginal opening.
- Enterocele: the small intestine bulges against the back vaginal wall.

What are the symptoms of a prolapse?
Pelvic organ prolapse symptoms include:
- A feeling of heaviness around the lower abdomen and vagina
- A dragging discomfort inside the vagina
- Feeling like there's something coming down into the vagina – it may feel like sitting on a small ball
- Feeling or seeing a bulge or lump in or coming out of the vagina
- Discomfort during sex
- Problems going to the toilet, such as feeling like the bladder or bowel is not emptying fully, needing to go more often, or leaking pee when coughing or exercising (stress incontinence)
What can cause a vaginal prolapse?
The main cause is from damage to the nerves, ligaments and muscles that support the pelvic organs this may occur due to:
Pregnancy and childbirth
These are considered to be major factors that can lead to weakening of the vagina and its support. Prolapse affects about one in three women who have had one or more children, prolapse can occur during, shortly after or decades after pregnancy. If a woman has had numerous vaginal deliveries, a long labour, or a big baby, the chance of prolapse may be higher.
Menopause
Oestrogen has a crucial role in maintaining the strength of the pelvic support structures. The lack of oestrogen during menopause, weakens the support structures and tissue that hold pelvic organs in place.
Surgery
Vaginal and vault prolapse is more common in people who have undergone a hysterectomy , (removal of the uterus and cervix). This can be because the supportive ligaments have been released during surgery.
Getting older
Your risk of prolapse increases with age.
Genetic or hereditary factors
The pelvic support system could naturally be weaker. Some diseases such as Marfan syndrome or Ehlers-Danlos syndrome affects the strength of the connective tissue.
What is the treatment for pelvic organ prolapse?
- No treatment: prolapse is not a life-threatening condition and some women choose not to have any treatment, especially if they have no symptoms or discomfort.
- Exercise: kegel exercises are a type of exercise that strengthens the pelvic muscles, these can help with minimal or mild prolapse.
- Vaginal pessary: a vaginal pessary is a device that sits in your vagina and typically looks like a little plastic or rubber doughnut. It serves as a structural support keeping organs or tissues in place. More information about this treatment, and the types of pessaries, is available in our services section.(link)
- Lifestyle changes: these can include losing weight, avoiding heavy lifting, and preventing constipation.
- Intravaginal laser: laser therapy can be used in mild prolapse to stimulate collagen production resulting in re-strengthening of the vaginal tissues.
Surgical treatments
- Hysterectomy: hysterectomy is a surgery involving removal of the uterus and cervix. This can be done as a vaginal or abdominal approach. Most prolapse surgery would be performed vaginally. After the hysterectomy is performed the surgeon will assess if you require vaginal reconstruction as well.
- Vaginal reconstruction: this may also be known as an anterior (front vaginal wall) repair or a posterior (back vaginal wall) repair. The patient’s own tissues along with non-permanent stitches are used to re-strengthen the vaginal walls, replacing the pelvic organs into their original position.
- Sacrocolpopexy: a piece of mesh is fastened to the vagina and secured to the tailbone to raise the vagina. More information about this treatment are available in our services section.
- Vaginal vault suspension (sacrospinous ligament fixation): with this treatment the vagina is connected to the strong, supportive ligaments in the pelvis.
- Tolpocleisis: this entails closing the vagina with stitches, resulting in the low risk of developing another prolapse. This is not suitable for patients that want to retain a vagina for penetrative intercourse.
This content has been reviewed by Susan Wilson, Gynaecology Fellow SPR Obstetrics and Gynaecology in Women’s Health at our Centre for Women's Health in Cork.