Macular Degeneration
What is macular degeneration?
Macular degeneration can affect one or both eyes and is a very common cause of reduced vision in Ireland. It affects central vision but not the side vision. Vision can be significantly impaired, however, in many cases it does not lead to complete blindness.
The macula is a part of the retina, the light sensitive layer at the back of the eye, which receives images and transmits them to the brain. It is responsible for central vision such as seeing fine details, reading, writing, interpreting colours, making out facial features and shapes.
With macular degeneration, the cells within the macula deteriorate which can cause varying amounts of blurred vision and varying loss of central vision. 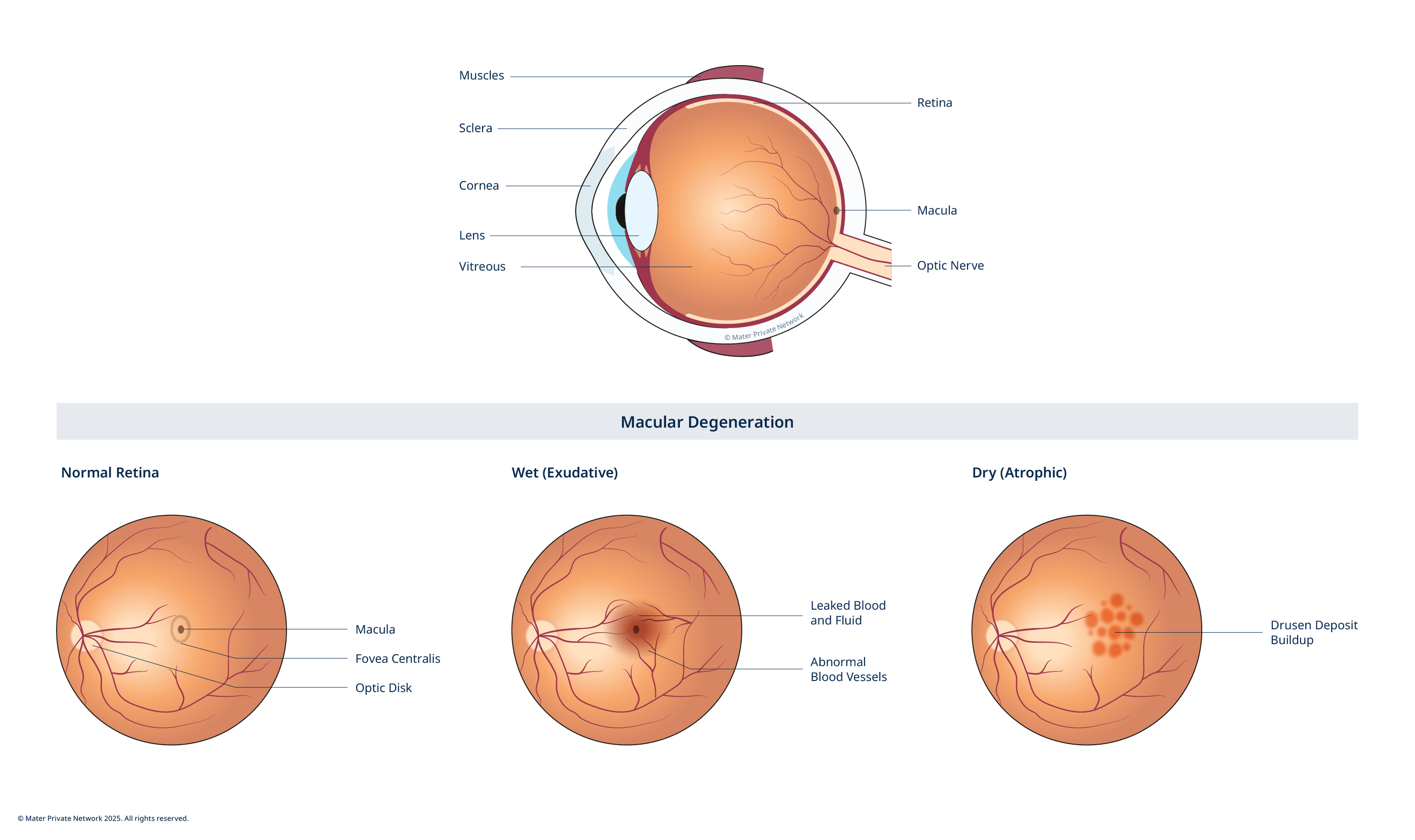
What are the causes of macular degeneration?
The exact causes of the condition are not known. It is thought that as we get older the macula degenerates (wear and tear) which causes the macula to deteriorate, therefore affecting vision.
Some contributing factors of macular degeneration include:
- Age
- Gender
- Diet
- Light exposure
- Family history
- Obesity
- Diabetes
- Heart disease
- High blood pressure
- Smoking
What are the different types of macular degeneration?
There are 3 types of macular degeneration:
- Dry macular degeneration: this is the most common type accounting for 80-90% of all cases. This may occur when cells in the macula break down overtime, gradually blurring central vision. Patients may have difficulty recognizing faces and may need more light to read and perform other tasks. Over time, dry macular degeneration may develop into wet macular degeneration.
- Wet macular degeneration: this may occur when abnormal blood vessels behind the retina grow under the macula. These new vessels are very fragile and leak fluid. The fluid raises the macula from where it normally lies which may cause vision to become distorted with straight lines becoming curved or wavy. Some people will also see a blurred spot in the centre of their vision.
- AMD: age-related macular degeneration (AMD) is a condition affecting the eyes as you get older. In Ireland, AMD is the leading cause of sight loss in the over 50’s and is more common in men than women. There are over 7,000 new cases in Ireland every year.
What are the symptoms of AMD?
A person with AMD is likely to have varying degrees of vision problems such as:
- Distortion – images or straight lines may appear wavy or bent
- Dark patches or empty spaces – black hole in the centre of vision
- Difficulty in reading or doing any other activity which requires fine/detailed vision
- Difficulty in distinguishing faces
End-stage AMD
End-stage AMD is the most advanced form of the disease. It can result in severe loss of central vision sight. Side vision or peripheral vision, is not affected by AMD. However, due to the low resolution or quality of sight it provides, it is not enough to compensate for the loss of central vision. Unfortunately at present there are no drugs or treatments available to cure end-stage AMD.
What are the symptoms of end-state AMD?
- Central blind spot – often described as a black hole in the middle of their vision.
- Difficult or impossible to see faces or read.
- Difficulty with everyday activities such as watching TV, preparing meals, dressing, shaving, applying makeup.
How is end-stage AMD diagnosed?
Generally an optician or GP are the first to detect the signs of macular degeneration in a patient. These could be such changes as "black spots" appearing in your line of vision or if you are seeing what should be straight lines as broken or distorted.
If macular degeneration is suspected, you will be referred to a retinal consultant specialist where further testing will be carried out.
At Mater Private Retinal Clinic a variety of examinations are used for the diagnosis of retinal conditions such as macular degeneration incuding:
- Visual acuity: measures how well you see at various distances.
- Slit lamp examination: examines your eye under high magnification.
- Tonometry: measures the pressure in the eye.
- Eye examination: where drops are used to dilate the pupil and examine the retina in detail.
- Amsler grid: a lined grid used to check for distorted or missing lines.
Following these initial tests, a series of retinal examinations will be carried out in order to investigate what damage, if any, macular degeneration has caused:
- Color fundus photography: photography of the fundus (inner lining of the eye) to produce a sharp photograph of the retina and the blood vessels.
- Fluorescein angiogram: where a special dye injected into a vein in the arm, as the dye passes through the blood vessels in the retina a photograph of the eye is taken.
- Indocyanine green angiography: similar to the fluorescein angiography, using indocyanine green dye.
- Optical coherence tomography: 3D scans of the layers of the macula part of the retina.
What treatments are available for macular degeneration?
A combination of treatment and lifestyle measures are used to help manage and treat the effects of macular degeneration:
- Telescopic lens implant: is the latest treatment option available to patients in Ireland with AMD. The programme is led by consultant ophthalmologist, Prof David Keegan at Mater Private. Prof Keegan is the first surgeon in the island of Ireland to offer this surgical option to patients as part of the CentraSight care programme. The tiny telescope is implanted inside one eye, behind the iris (the coloured part of the eye). Smaller than a pea, the telescope implant uses micro-optical technology to magnify central vision images – “straight ahead” vision.
- Laser: used to destroy the fragile leaky blood vessels.
- Injections: used to block the effects of the growth of new fragile blood vessels. This can help to slow down vision loss. More than one injection may be needed.
- Nutrition: fruits and green leafy vegetables are recommended as a healthy diet can slow the progress of AMD.
- Sunlight: it is recommended that you reduce exposure to sun light and wear sun glasses.
- Smoking: stop smoking as smoking can accelerate the progress of macular degeneration.
- Monitor vision daily: using the Amsler grid or something with a fixed, straight line like a bathroom tile or street light.
- Low vision aids and lighting: won’t halt the progress but will improve quality of life, e.g. using magnifiers for reading.
- Antioxidant supplements: such as lutein, beta carotene, vitamins C and E, and zinc or vitamins. This should always be discussed with your consultant first before commencing any new medication.









