Testicular Cancer
Is testicular cancer common and what symptoms should I look out for?
On average there are more than 170 men diagnosed with testicular cancer each year. This cancer is known to be most prevalent between the ages of 15 – 35 years of age.
Doctors recommend that a self-check is done monthly in order to detect any abnormalities of the testicles or scrotum and this is recommended following a hot shower each month.
An abnormality is where you might find the following:
- A lump in one or both testicles or scrotum.
- Pain or numbness in the testicles or groin area.
- The difference in the weight of either testicle, when one testicle is heavier or lighter than that of the other.
What should I do if I find any abnormalities?
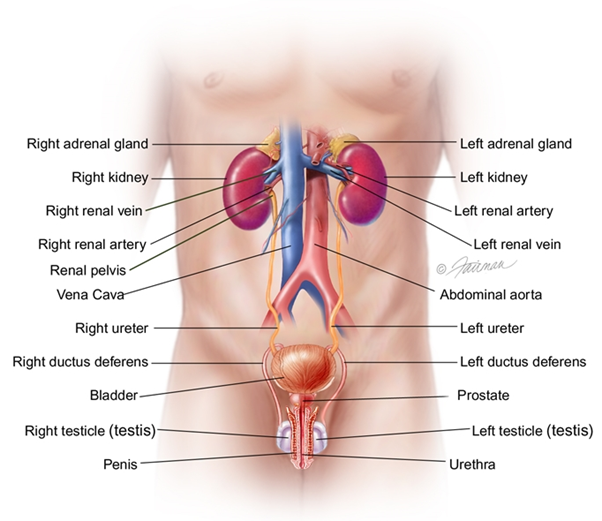
If you find any abnormalities, it is recommended you visit your GP where your general medical health will be discussed and your past medical history noted. Your GP will refer you to a consultant urologist for further evaluation. A consultant urologist is a doctor who specialises in disease of the urinary tract. During your consultation your urologist will looks for evidence of enlarged lymph glands in your armpits, neck, under arms, chest and groin area. He will look for any leg swelling or growth and tenderness in the area of your breast. Your urologist will most probably want you to have an ultrasound, blood tests to determine if the abnormality is benign (non cancerous) or malignant (cancerous), and a CT scan.
Ultrasound
An ultrasound is a way for your consultant to find any lumps or abnormalities within the testicles or scrotum area. If a lump is found then the ultrasound will be able to determine the size and location and confirm if it is a solid lump.
Blood tests
Your blood will be examined to look at proteins and hormones (tumour markers) that are linked to testicular cancer.
CT scan
A CT scan is used to evaluate the chest, lungs, abdomen and other areas using x-ray images of inside the body from difference angles. A computer defines these images into detailed three dimensional images of the body.
What are the types of testicular cancer?
There are two main types of testicular cancer:
Germ cell tumors
- Embryonal carcinoma
- Yolk sac carcinoma
- Choriocarcinoma
- Teratoma
Stromal tumors
- Leydig cell tumors
- Sertoli cell tumors
What treatments are available?
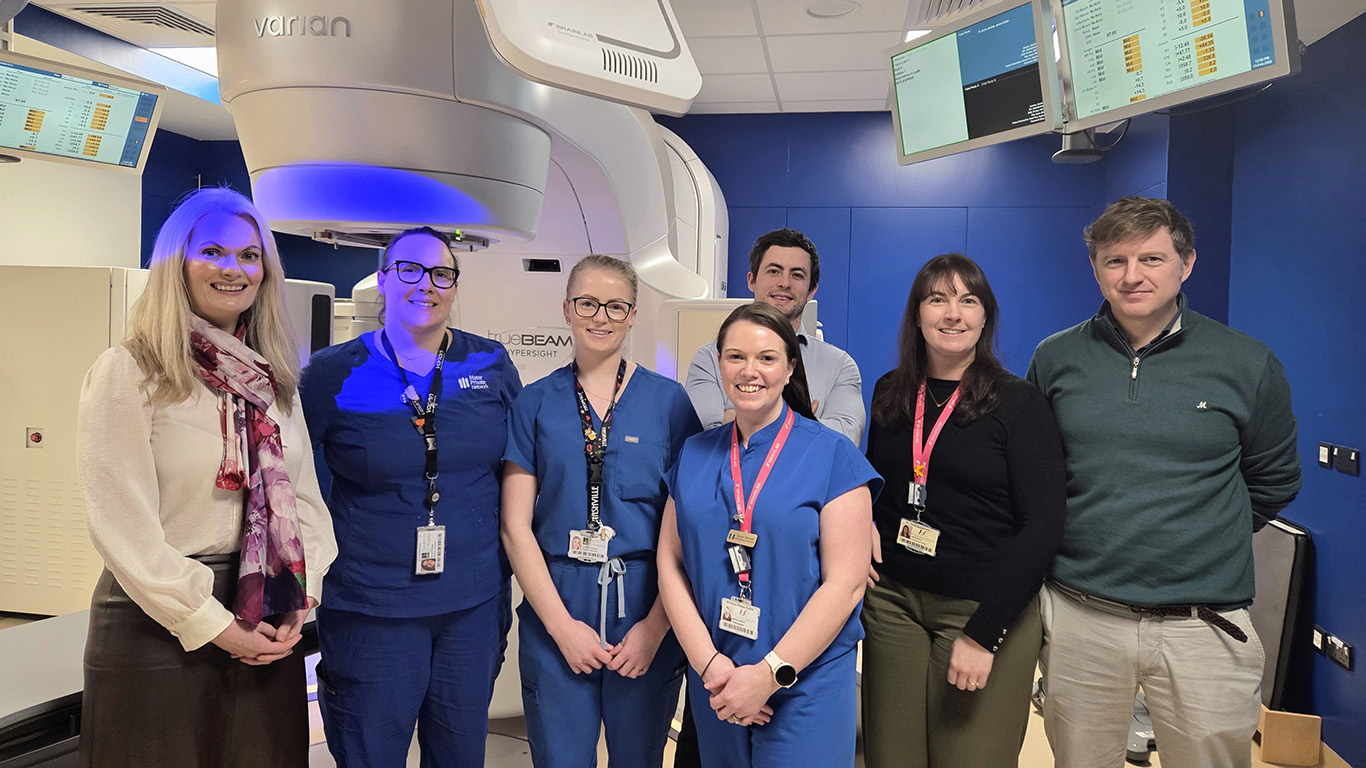
Following your diagnosis, you will be referred to an oncologist, where your treatment plan and schedule will be discussed with you in detail. Every treatment plan is specifically devised for each patient individually, and include radiotherapy, chemotherapy and surgery. The side effects from radiotherapy and or chemotherapy can be discussed with your consultant oncologist.
Chemotherapy
- These are high powered drugs given through IV infusions which kill cancer cells.
- This is typically cisplatin and etoposide and possibly bleomycin. The vast majority of patients are cured of this disease.
What to expect:
Before your treatment starts you will have discussed your treatment plan with your consultant and will have received a schedule of appointments. On the day of your treatment you will be asked to attend our phlebotomy Department, where you will have some blood tests one hour before your treatment is due. When your arrive in the Cancer Centre day ward for chemotherapy, you will be greeted by the medical team and your nurse will be happy to show you around the day ward in order to familiarise yourself with it. She will discuss your bloods results with you and take your medical history. Please ask any questions you have with your nurse and she will be happy to answer them for you. You will be given light refreshments, tea/toast on the day. We recommend that you bring a book, newspaper and your earphones with you to help pass the hour’s easer for you.
If surgery is recommended, what does this mean?
If testicular cancer is suspected, a surgeon will perform a radical inguinal orchiectomy which is a procedure whereby the whole testical is removed through an incision in the groin. This procedure is done under general anaesthetic. A biopsy is taken from the tissue of the testicle and this will be examined by the consultant pathologist (tissue expert) to determine what type of cancer it is.
Prosthetic testicle
During surgery a prosthetic testicle can be inserted into your scrotum. These are silicone implants which are filled with salt water to enhance their natural appearance and ensure confidence after surgery. You can have a prosthetic testicle placed during your surgery or at a later time and this can be discussed in details with your surgeon. There are minor risks associated with the prosthesis and this can also be discussed with your surgeon.
Following your surgery:
- Normally you will be discharged from hospital two days following your surgery.
- Bruising or swelling of the scrotum after surgery is normal.
- You will be asked to abstain from any lifting heavy objects, excessive exercise or sport for three to four weeks.
- Most people will be able to return to a normal sex life after surgery.
- If you have any concerns in relation to your sex drive or feeling extremely tired, your consultant can discuss testosterone replacement therapy.
- Having one testicle removed does not normally effect your fertility, however you can discuss this in further detail with your consultant.
What happens after my treatment is finished?
Once you have finished your treatment, your consultant will let you know when you will be coming back to see him or her and how often this will occur. When you return, your consultant may want you to have blood tests, scans. During these visits your consultant will check for signs or symptoms that your cancer may have returned. Your consultant will also check for any side effects that you may have. Always remember, we are here to discuss any worrying symptoms you may have, and if you are in between your consultations please let your consultant know.
Will treatment affect my fertility?
Some treatment that you may have can affect your ability to father a child. This is a very important issue that should be discussed with your consultant, prior to starting your treatment. Sometimes, this can be an overwhelming topic to discuss if you are not ready to become a dad for the first time, and if it is something that you never had to think about until now. However, over time as the years and months go by, your feelings on this may change, therefore it is best to discuss this now, become prepared and visit all your options. There are many men who have gone on to father children following their treatment.
Sperm banking
As we know, testicular cancer is curable and it is because of this, that we encourage our patients to take the time to embrace their future and think about whether you would like to become a father. It is with that thought in mind that we discuss the topic of sperm banking.
What happens next:
Your consultant will advise on the various tests that are carried out on your sperm prior to starting your treatment, in order to see if you are infertile or if you have a low sperm count. If your sperm count is within normal limits, it may be possible to store your sperm before you start your treatment. Your sperm can then be used at a later date, as it will be frozen and stored. In order to do this you will be asked to give several sperm samples. There will be a break between samples and this is to make sure good samples are received. Sperm banking can be done in the HARI Unit at the Rotunda Hospital in Dublin and in some other fertility clinics around the country. One important factor to remember is that collecting sperm will not delay your treatment in any way, as this is done while you are waiting on other specific tests to be carried out and results reviewed by your consultant. This is all encapsulated as part of the process you are going through. Please do discuss this with your consultant or liaison nurse as they are happy to answer your questions.
If it happens during your cancer journey, that fertility issues arise this may bring sadness, anger, frustration and a loss of identity to you. You may also feel shy, embarrassed or anxious talking about such a personal issue. It will help if you raise these concerns with your consultant or liaison nurse, who can put you in touch with a specialist counsellor, who can be a confidential and compassionate listener to you.
"At the Cancer Centre we pride ourselves on always putting are patients at the forefront of everything we do, as we are part of your cancer journey. We understand that attending the Cancer Centre can be a stressful and anxious time for you, however please be assured that we are always available to answer any questions you may have in order to make you as comfortable as possible".