Prostate Cancer
I’ve been told that I have prostate cancer. What is it exactly?
Prostate cancer is the second most common cancer affecting men in Ireland. Almost 4,000 new cases are diagnosed each year and the incidence is increasing.
Regular prostate specific antigen (PSA) checks are really important for men over 50 as prostate cancer can be present for many years without even knowing it. PSA is a protein made by your prostate gland that naturally spills into your bloodstream. If your PSA level is higher than normal, it can sometimes be a sign of prostate cancer but often it can just be a sign of a less serious condition such as an enlarged or inflamed prostate.
At Mater Private, we continue to maintain our position as Ireland's leading prostate centre, offering the widest range of treatment available in any centre in Ireland. We are the only centre to offer all types of surgical and radiation therapy treatment for this condition.
What are the risk factors for prostate cancer?
- Age: rare in younger men. Risk increases when you are over the age of 50.
- Family history: risk increases if your father or brother had prostate cancer. If they had it at a young age, the risk is greater.
- Diet: eating a healthy diet can lower the risk.
- Weight: obesity or being overweight.
What are the symptoms of prostate cancer?
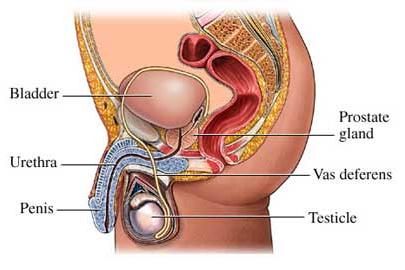
The prostate is located below the bladder and in front of the bowel. It surrounds the beginning of the urethra and the nerves that control erections. It produces fluid to protect and enrich sperm.
Symptom Checker:
- Urinating more often than usual
- Getting up a number of times during the night to urinate
- Difficulty urinating
- Pain when urinating
- Trouble starting or stopping urinating
- Bladder doesn’t feel empty
- Pain in the lower back, hips or upper thighs
- Trouble having or keeping an erection
- Blood in urine or semen
- Fatigue
The warning signs for prostate cancer are similar for a number of prostate problems, so while you might be worried about cancer, it may not be cancer. A simple PSA test carried out by your GP will help provide a more accurate diagnosis and set your mind at ease.
How is prostate cancer diagnosed?
If prostate cancer is suspected, a combination of tests will be carried out to confirm the diagnosis:
- Prostate specific antigen (PSA) test: this test is a blood test to identify the levels of a protein called prostate specific antigen. PSA levels are used as part of the information gathered to identify a possible prostate cancer.
- PSA is produced by both normal and cancerous prostate cells. A high level of PSA can be a sign of cancer. However, the levels can also be raised in prostate conditions that are not cancer or if you have an infection.
- PSA blood tests are also used to monitor how well prostate cancer treatment works or to decide whether you need treatment. If your PSA is stable, it is a sign that a cancer is not growing or spreading. Successful treatment shrinks cancer and the PSA level in the blood will fall.
- Digital rectal exam (DRE): PSA testing combined with DRE helps identify prostate cancers at their earliest stages. During a digital rectal exam your doctor will examine your prostate gland by gently inserting a lubricated gloved finger into your rectum. Your doctor can feel the surface of the prostate gland and check for abnormal signs, such as a lumpy, hard prostate. If your doctor finds any abnormalities in the texture, shape or size of your gland, you may require further tests.
- Rectal ultrasound: this is used to examine the prostate gland. It involves a small ultrasound device being put into the rectum (back passage) to generate a picture of the prostate gland. This test is uncomfortable, but should not hurt.
- Prostate TRUS biopsy: TRUS stands for transrectal ultrasound. The ultrasound is used to take an image of the prostate gland and allows a small sample of cells to be taken accurately during the biopsy. The ultrasound probe is inserted into the rectum and the biopsy is taken through the thin rectal wall. In general, sedation is not required and the procedure is well tolerated with a local anaesthetic. This test can determine if you have prostate cancer and can indicate how quickly it may develop (grading).
- PCA 3 urine test: the PCA3 test is a new type of test, which doctors hope will help them to determine more efficiently who may have prostate cancer and require a biopsy. PCA3 stands for prostate cancer gene 3. Prostate cells have PCA3 genes which make the cell produce a small amount of a particular protein. Prostate cancer cells create more of this protein than normal cells. When the level of PCA3 protein is high, it leaks into the urine.
- The PCA3 test is not yet accurate enough to be used on its own as a test for prostate cancer. It is more likely to be used in combination with a PSA test, to help your doctor decide whether you need a prostate biopsy.
- The PCA3 test is not yet accurate enough to be used on its own as a test for prostate cancer. It is more likely to be used in combination with a PSA test, to help your doctor decide whether you need a prostate biopsy.
What is prostate cancer grading?
Once testing is complete, your doctor assigns your cancer a stage. This helps determine your treatment options. The prostate cancer stages are:
Stage 1 - the cancer is very small and completely inside the prostate gland which feels normal during a rectal examination.
Stage 2 - the cancer is still inside the prostate gland, but is larger and a lump or hard area can be felt during a rectal examination.
Stage 3 - the cancer has broken through the covering of the prostate and may have grown into the tubes which carry semen.
Stage 4 - the cancer has grown into the bladder or rectum, or has spread to the lymph nodes.
What treatments are available for prostate cancer?
Your prostate cancer treatment options depend on several factors - how fast your cancer is growing, how much it has spread and your overall health, as well as the benefits and the potential side effects of the treatment. What type of treatment you are recommended, will depend on the type of prostate cancer that you have been diagnosed with:
Low risk localised prostate cancer
- Prostate cancer is very unlikely to grow or develop for many years.
- In older men, they are likely to be offered active surveillance.
- In younger men may, they may be offered prostatectomy or brachytherapy such as radioactive seed implantation.
Intermediate risk localised prostate cancer
- Prostate cancer may start to grow or spread within a few years.
- Treatment usually offered is surgery to remove the prostate gland or radiotherapy to the prostate.
- Active surveillance and/or hormone therapy may be also considered.
High risk localised prostate cancer
High risk prostate cancer patients are likely to be offered surgery to remove the prostate gland and/or external radiotherapy to the prostate. Internal radiotherapy (brachytherapy) is not often used, because in high risk prostate cancer the cancer cells may have spread slightly away from the prostate gland and internal radiotherapy may not reach all of the damaged cells.
For men who are not fit enough to have radiotherapy or surgery, a doctor may recommend active monitoring as a treatment option.
Locally advanced prostate cancer
This is cancer which has broken through the capsule surrounding the prostate gland. For locally advanced prostate cancer, surgery to remove the prostate gland or external radiotherapy to the prostate may be combined with a course of hormone treatment. Hormone therapy may be used before surgery or radiotherapy, or afterwards for up to three years.
Men who cannot have surgery or radiotherapy because they are not fit enough, may have a course of hormone therapy as a treatment on its own.
Treatment options
Active surveillance
Active surveillance is a monitoring of the cancer to see whether it begins to develop. This is because your prostate cancer may be growing so slowly, that it never causes any symptoms or effect your quality of life.
Prostate cancer specialists use monitoring because they know that some men with prostate cancer will never need treatment. Treatments for prostate cancer can cause long-term side effects, so doctors try to avoid giving treatments if safe to do so, as the benefits outweigh the risks.
Regular blood tests and checks are carried out during active surveillance to monitor if there are any changes to the cancer. Treatment can be started straight away if there is any sign that your cancer is beginning to change or grow.
During monitoring, there are some things you can do which may help to keep you healthy and will help you to feel you are doing something positive:
- Eat a healthy diet
- Learn to relax
- Stop smoking
- Take notice of any new symptoms and report them to your doctor
Hormone therapy
Hormone therapy is used to treat prostate cancer by stopping testosterone being released or by preventing it from stimulating the prostate cancer cells to grow. It it most effective in the treatment of localised prostate cancer. It can also be used in men who are not suitable for other forms of treatment such as surgery or radiotherapy due to their age or poor general health. In the case of locally advanced prostate cancer, hormone therapy can be used to reduce the risk of the cancer spreading further.
Hormone therapy options include:
- Medications that stop your body from producing testosterone.
- Medications that block testosterone from reaching cancer cells.
- Surgery to remove the testicles (orchidectomy) as this will reduce testosterone levels in the body.
Radiotherapy
Radiotherapy uses radiation to damage cells and stop them from growing and dividing. The aim of radiotherapy is to destroy the cancer cells while minimising the damage to the normal cells.
If your prostate cancer has spread to the bones and is causing you pain, your specialist may suggest using radiotherapy to treat the affected areas of bone. It can help to strengthen the bone and relieve pain. The damaged bone begins to repair itself after radiotherapy treatment is complete.
There are three possible ways in which radiotherapy may be delivered for the treatment of prostate cancer:
- External beam radiotherapy
- Intensity modulated radiation therapy
- High dose rate (HDR) brachytherapy
Prostate seed brachytherapy (RASI)
Your consultant will decide which type of radiotherapy is most appropriate for you. Some patients may receive more than one type of radiotherapy treatment and it can also be used in conjunction with other treatments such as hormone therapy.
Chemotherapy
Chemotherapy may be a treatment option for men with prostate cancer that has spread to distant areas of their bodies or if they have not responded to hormone therapy.
For men, despite its effectiveness at destroying this type of cancer, either the cancer itself or the chemotherapy may cause permanent or temporary infertility. However, it is possible to store your sperm before treatment begins and this is something that can be discussed with your doctor in advance.
Surgery
1. Prostatectomy
A total or radiacal prostatectomy is a procedure used to remove the entire prostate gland,seminal vesicles and in some cases the lymph nodes. The aim of a radical prostatectomy is to treat (or cure) early prostate cancer, where the cancer is still within the prostate gland.
The operation can be performed using a number of different techniques:
- Open surgery - is performed in one of two ways. The standard approach is through a midline incision in the abdomen from just below the belly button (umbilicus) to the top of the pubic bone. The second way is through an incision in the area behind the scrotum called the perineum. However, this is now a very rarely used approach.
- Laparoscopic assisted keyhold surgery - during a laparoscopic radical prostatectomy, the doctor performs surgery through small incisions in the abdomen with the assistance of a tiny camera (laparoscope). At Mater Private, radical prostatectomy is now only performed by the robotic-assisted minimally invasive approach.
- Robotic assisted surgery - thanks to a breakthrough surgical technology, Mater Private now offer a minimally invasive option for prostatectomy, the da Vinci prostatectomy. During robot-assisted surgery, the instruments are attached to a mechanical device (robot) and inserted into your abdomen through several small incisions. The surgeon sits at a console and uses hand controls to guide the robot to move the instruments. Patients having robotic prostatectomy on average return to normal activity in 6 weeks versus 12 weeks with traditional surgery and have an average length of stay at hospital of 2.9 days. They will also experience less blood loss.
Download the Prostatectomy Patient Information Leaflet
2. Orchidectomy
Orchidectomy is the removal of both the testicles so that they cannot produce testosterone any more as testosterone can make prostate cancer grow. This operation is not commonly used these days, as hormonal therapies that stop the testicles producing testosterone are usually used instead.
3. Trans-urethral resection of the prostate (TURP)
This involves the removal of the inner area of the prostate gland around the urethra, the tube that carries urine from your bladder. This operation is not to cure or remove prostate cancer but it is done to relieve symptoms such as being unable to pass urine.
Living with prostate cancer
For many men, the treatment for prostate cancer can cause side-effects and problems. It is advisable to ask your doctor before you start treatment what side-effects you can expect, how to cope with them and what options there may be to ease them. Some of the issues that you may experience during treatment are outlined below:
- Sleep: if you are feeling worried and find it hard to sleep at night, speak with your doctor or nurse for advise on how to improve your sleep pattern. Although you may not normally nap during the day, don’t try to beat the tiredness and take a nap if you feel you need it.
- Talk: try talking to your close family or friends about your concerns – a problem shared is a problem halved. If you find this difficult ask to see a counsellor and he or she will help you to find ways to relax.
- Exercise: it you are able to, exercise can help. A 10-minute walk, three days a week might be a realistic goal and will boost your morale when you achieve it.
- Eating and drinking: you may notice that you have lost weight. This may be due to the cancer or the treatment you are getting. Sometimes when you are feeling weak and tired you may lose interest in your food. Ask for help in preparing your meals. Eat your favourite foods and drink lots of clear fluids such as water and fruit juice.
- Fatigue: fatigue is a common symptom of cancer and is often described as an overwhelming tiredness. You may find it difficult to concentrate or make decisions. Anxiety and stress can add to the feeling of fatigue. Remember that even though you may find it hard to identify the reasons for your tiredness, there are things you can do to help.
- Erectile dysfunction: treatment to the prostate gland can lead to problems in having an erection. This is called erectile dysfunction or impotence. Impotence may also occur as a result of increased anxiety or other medical problems (such as high blood pressure, diabetes and heart disease) and means that a man can’t get an erection strong enough to have sex. Any type of treatment may make you too tired to be interested in sex. This is known as loss of libido and it is common to many illnesses, not just cancer.
- You may find it difficult to talk about such personal subjects as erectile dysfunction, particularly with your doctor or other healthcare professionals. Try not to be embarrassed as the doctor and other healthcare professionals looking after you will be happy to discuss any concerns you may have. Impotence may not be permanent and can sometimes be brought on by anxiety rather than the treatment. Depending on the treatment you receive, it can take up to a year before you find out if the erectile dysfunction is permanent or not.
- If you find the loss of your sex life upsetting, you could discuss this with your doctor or nurse. There are practical ways such as medication to overcome erectile dysfunction and your doctor can give you further information about these.
- Infertility: some cancer treatments, and sometimes the disease itself can cause infertility. This may be permanent or temporary. You should discuss the possible risk of infertility with your doctor before you start your treatment. For men, the cancer itself or the treatment can cause infertility, this may be temporary or permanent. It may be possible to store your sperm before treatment begins and this can be discussed with your doctor when recommending your treatment for prostate cancer.